
Background: 1973 surgery, 2012 pain onset
In the fall of 1973, I had cartilage removed from my right knee. The cause of the damage was a fall while cross-country skiing the previous winter. Now, at age 63, I have had a good 41 years despite the missing parts (2:47:00 marathon, 100-mile running races, mountaineering, climbing, ski mountaineering, desert backpacks, lots of nordic ski racing), but for the past two years my knee gets inflamed on certain activities (mostly downhill walking). The cause is the bone-on-bone situation, and so it is time to get plastic cartilage and metal ends to the femur and tibia: total knee replacement.
The pain I had was an inflammation near the popliteus muscle. It started about January 2012, and I recall some bad days on a ski ascent/descent of Mt. Field in B.C. in April 2012, and, especially, on an 18-mile walk to Perseverance Arch on May 1, 2012. So it took 2.5 years for me to reach this point of deciding on surgery.
I first saw Dr. Cunningham in July 2013; I had had an MRI and consultation with an orthopedist in St. Paul in Nov. 2012, though that did not lead to a definitive diagnosis. Dr. C. gave me a cortisone shot, which worked well for a few weeks (and which confirmed his diagnosis). Fall 2013 was bad. Winter 2014 was fine. A Synvisc shot in April 2014 provided no relief at all.
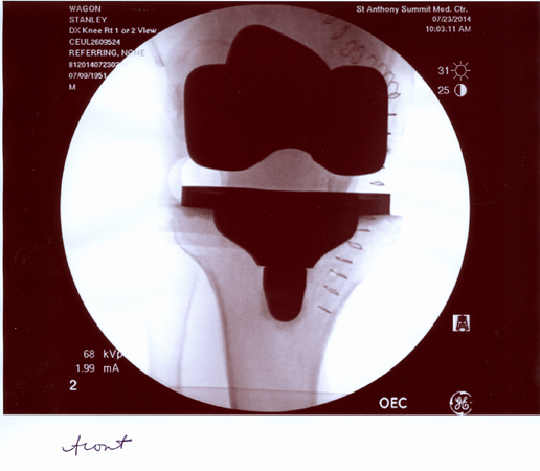
Here is a picture, from the front, of my right knee (Oct 2012). The spacing on the medial side (lookers right) is down to 0.
Compare with the spacing with the artifical knee, in the pics section below.
Notes for Distant Future
Take antibiotics before any dental work or minor surgery until July 23, 2016. This includes routine teeth cleaning.
An xray five years post-op likely will show nothing, so nothing is really needed until ten years, assuming all works well. I had an xray in 2021 and it showed no change from 2014. I write this in 2025 and my new knee is by far my stronger knee.
July 15, 2014: The pre-op discussion day
Pre-op meeting with surgeon, Dr R. Cunningham of Vail-Summit Orthopedics, his assistant Matt Cain, and anesthesiologist Dr. Peterson. New Xrays were taken.
Dr C. says that, although it might be possible to treat my problem with a partial knee replacement, he thinks total is best in my situation. It will be somewhat preventative re arthritic issues related to the kneecap. He described the device he will install (Stryker Triathlon). It gets cemented to the bone. Metal is CoCrMo: cobalt-chromium-molybdenum; a plastic piece serves as the cartilage replacement. And there will also be patellar resurfacing: a plastic piece cemented to the patella.
Good news: my other leg shows no problem.
Current flexion on right is 125°–130°. Current extension was measured at about 4°.
Discussion of activity choices once recovery is complete is delicate. E.g., downhill running is strongly discouraged. But how to define “downhill”: Peaks Trail vs running down Quandary? And what about downhill skiing at ski areas? I do that rarely so probably it is not an issue, though hard and regular area skiing is likely discouraged. They will check the implant in the future to see how much wear there is. But Dr. C says that likely little wear will show at five years, and a check at ten is reasonable. But he is willing to see me after five!
Anesthesia choice is tricky. There are two choices. Anesthesiologist prefers a spinal block together with a drug that puts me to sleep. Reason: Morphine can be introduced; recovery is easier. But Dr C. just responded by email that he prefers the general because the spinal immobilizes the leg for longer and he wants activity and movement ASAP. So I will follow his advice.
The hospital stay will be one, two, or three nights, depending on progress (turned out to be three). The post-op rehab program is extremely important, as scar tissue will build, and it must be broken down by exercises. I will do my best. Also the angle my foot bends backward will likely increase by a few degrees. Of course, the main question is: After his procedure, will my current pain, caused by bone-on-bone on the medial side, disappear. One hopes so. That is part of the rationale for the total, since it would be sad if I had a partial done and the pain remained.
VSO is headquartered in Vail, but has a big office here at the Frisco hospital (St. Anthony Summit Medical Center, below), built in Frisco in about 2007. The hospital has about 35 beds.

July 17, 2014: Thinking
Naturally I spend a lot of time thinking about the surgeon’s recommendations for activities after I recover. His initial comments were: hiking (up and down), running (especially uphill), and nordic skiing are fine, but avoid downhill running. Downhill skiing is fine, but avoid the steepest runs. The main issue is deterioration of the plastic cartilage between the metal parts. If that wears down, a surgical “revision” might be needed. XRays can indicate wear, and they will be taken from time to time (5 years? 10?). Dr. C says that at 5 years there should be little or no wear.
My view is that, among all my activities, there were some that irritated my knee and some that did not. The irritation was inflammation due to the bone on bone. So it seems logical to me that activities that did not so irritate the bone will not be putting stress on the plastic cartilage. So, yes, downhill running is to be avoided, but the definition of “downhill” is vague. Trails such as the Peaks Trail or Mesa Cortina Trail are much different than running down Quandary. I have found that alpine (and backcountry) skiing did not stress my knee at all (except for one memorable day in bad conditions on Mt. Field in B.C.). So since I do only 5-6 alpine days a year, most of which are half-days, I imagine that a change in that practice is not really necessary. The web page of a large orthopedic outfit in Aspen suggests that this sort of skiing is not a problem.
July 21, 2014: Preparing
Nice long hike yesterday on fairly easy ground to Mt. Blaurock (13600) and neighboring unnamed, slightly higher, peak to the west, out of Winfield, Colo. Knee felt fine except for the usual last thousand feet of descent. But it was not an overly taxing hike.
The prep. for surgery involves showering on four consecutive days, including the morning of the surgery, with a cleansing chemical soap. Not a problem.
A neighbor came over and said that a new technique for total knee replacement is to make the initial cut on the side, instead of straight down the middle. She thought recovery was quicker with this entry. Hah! Because of my medial scar from 1973, the surgeon is planning to go in through that same scar! They don’t like parallel incisions within 7 cm, so this is how that is avoided in my case.
July 22, 2014: 12 hours to go
Nothing new. There is just enough little pain in my knee to convince me I am doing the right thing, especially as I exercised only very lightly today and yesterday.
July 23, 2014: Wednesday, S-day
The surgery went smoothly. Strangely I could not get the plot of NEVER LET ME GO (Kazuo Ishiguro novel — truly brilliant) out of my mind. Dr. C. got out of a meeting early and was able to move the time up from 9 to 8:30. The anesthesiologist (Dr. B) agreed that general was appropriate: he said it was good to avoid injections into the spine. He gave me the two nerve blocks: popliteal block and an adductor block (basically femoral and sciatic). They try to bathe the nerve in the drug, without touching the nerve, using an ultrasound to guide their needle close to the nerve, without touching it. Dr. C. dropped by briefly, and pretty soon I was unconscious. I remember being wheeled into the OR, but that is about it.
Recovery was ok: no nausea, tears, or combativeness. Then up to Room 211 for my, I hope, two-night stay [ended up staying 3 nights]. Dr. C. came in at some point. I like him and his manner, though I suppose every patient likes the surgeon after a successful operation. The op. took at most 75 minutes. He cut off about a quarter inch of bone on either leg bone, and also trimmed the osteophyte (bone spur) that had formed on the medial side. The ACL and PCL are removed. He cut through one tendon but then sewed it back together. He did say that there was no question I needed the surgery. Bones were touching and affecting each other, though not grinding. He also straightened the leg and said that that might make me feel a little taller. The actual sizing of the implant is designed to preserve one’s height, despite the insertion of plastic cartilage that was not there before. He did two of these surgeries today.
Amazingly only 50 mL of blood were lost during surgery; that’s all of 3 tablespoons. Also they cut through one tendon at some point and sew it back quickly; interesting.
Della Crone of PT (whom we knew from Joan’s surgery 16 months ago) came in and after a while we tried getting me to the bathroom. I got there ok, and was able to urinate, but both took an effort and I almost fainted on return. They got me to a chair, and then, eventually, to the bed. I feel fine now (8 pm), but will not try to exit the bed until tomorrow. So one small step back there, but still all goes well.
I had a good appetite at dinner, and a second urination into a container was easier than the first. I still can feel nothing below the right knee. That can take 24 hours to normalize.
This surgery was first done in 1954. Wikipedia has a link to the paper describing the first such surgery,
July 23, 2014: Pictures of the new knee
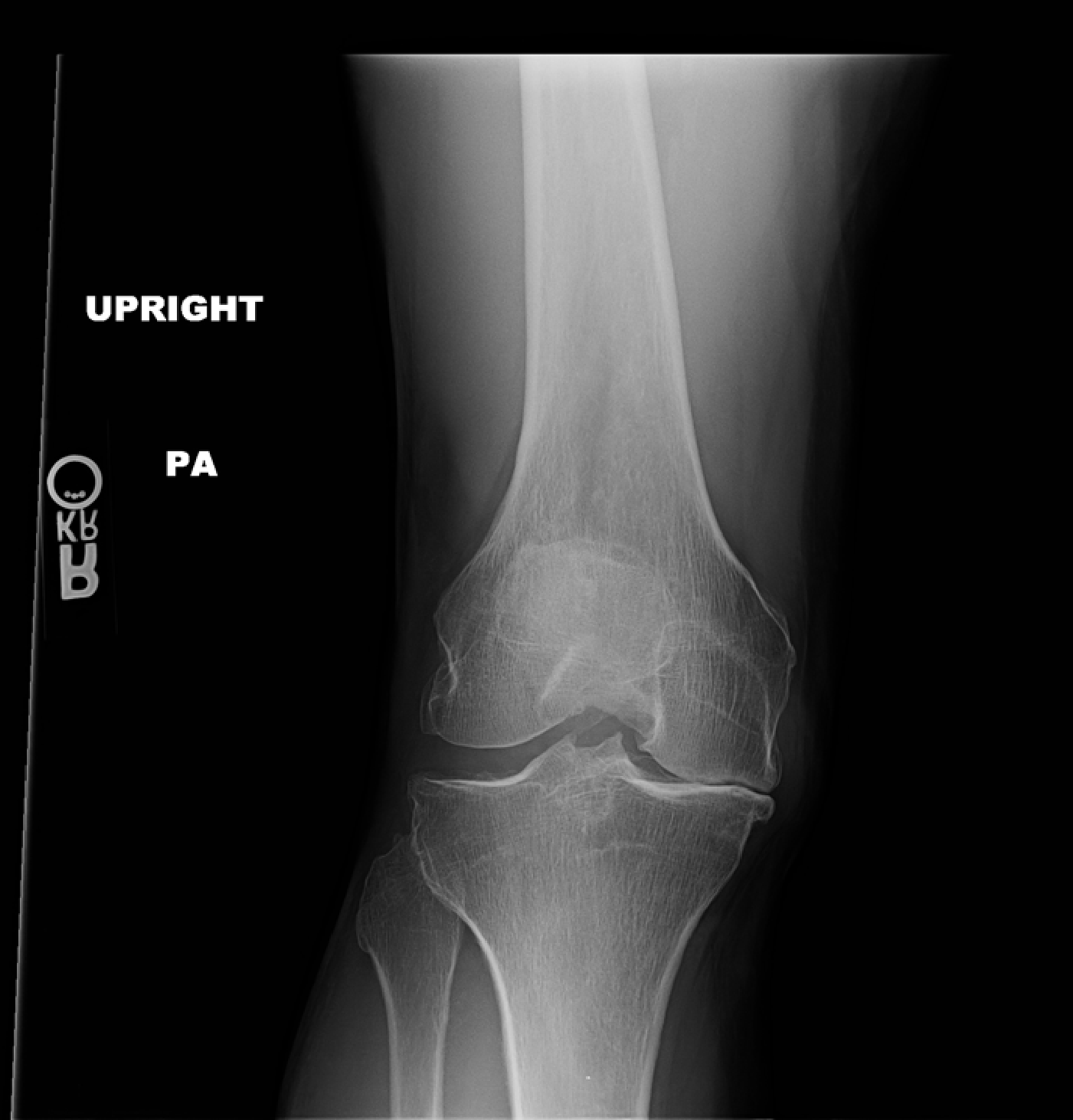
Here is the view from front to back. The space between the implants is occupied by plastic (polyethylene), which takes the place of cartilage. This is the spacing that a good knee shows, and which I did not have. The staples are on the inside (medial) of the leg.

And this is the side view, anterior to medial. Kneecap at left. Bone at right is the other leg. Patella at upper left. Fibula is visible, but the knee connects femur with tibia. There is more to the implant than one can see. Posts fix the pieces in place, and make the removed ACL and one other ligament irrelevant for stability. And a plastic piece is attached to the inside of the patella.

July 24, 2014: Recovery day in the hospital
Slept off and on during the night. Blood pressure was very low at every measure but finally at 7:30 am, there are 3 digits to the upper number! I am no longer on an IV for fluids. The anesthesiologist came by to figure out best plan for pain management, and suggests oxycontin instead of oxycodone. The block started wearing off to where I could wiggle my toes about 4 am, or after 20 hours. As to how much pain will now arise we will see.
Night nurse was Dori Welch, daughter of famed avalanche investigator/forecaster Nick Logan, who lives in Breckenridge.
10 am: Moved to a chair for the rest of the morning. Learned the first set of exercises to do.
3 pm: just finished good PT session; able to walk 200 ft. with crutches. Got a “Game Ready” ice machine that we will rent for 2-3 weeks. My quad is not working: I cannot lift my leg even a paper width. It appears to be a consequence of the general invasion of the leg (as opposed to the adductor block not wearing off, as it would have worn off by now). Naturally I hope this improves tomorrow.
7 pm: A good day of PT and I walked 200 ft on crutches, so I will likely go home tomorrow. But the problem with the dead quadricep seems a bit more serious. Dr. JB was concerned this morning (I could tell from his manner), and many phone calls and discussions were made in the afternoon among the anesthetists and Dr C (traveling to New York). Dr DL ( a senior anesthesiologist) just came in to explain his view of what happened. The femoral block consists of a block of the saphenous nerve, but NOT the femoral nerve which controls motor function. This change is something they have been doing for three months. DL feels that the damage to the femoral nerve was caused by the tourniquet. Had they blocked the femoral nerve, they might not be certain, but because they do not do that, he has no doubt that the tourniquet is the culprit. Of course, it makes sense as he put it all very logically. Some people have nerves that are more sensitive or placed more sensitively to this procedure.
It affects only the quadricep. He says it will revive in a few weeks. Certainly this will slow down my recovery. There is nothing to be done but watch it and hope it slowly improves.
My evening session on the CPM (continuous passive motion) had lots of pain. Now using cooling machine (Game Ready); it helps a lot.
July 25, 2014: Friday: Record low blood pressure 75/48.
8 am. Lots of pain on the evening exercises. Lots of urine production at night, which is normal as the IV liquids start to exit the body. A teeny bit more quadricep movement in the morning. Dr. L came by and was pleased by that. He reported that the tourniquet was on for only 45 minutes. This is relevant to how much nerve damage was sustained. So total surgery time was probably an hour. He reported that in phone call to Dr C., Dr C. said that really the surgery all went very smoothly. So now I have to hope for continued slow improvement.
At 10 we tried a walk and I did poorly. Dizzy. Blood pressure of 75/48, which is ridiculously low. Back to bed, got the CPM going — no pain — and a nap. I might have been dehydrated.
Hematocrit has risen from 30.8 to 31.9. That is low, but normal as body rebuilds red cells.
JB came in again as he administered the blocks and is concerned. He was very happy to see a bit more quad function, so maybe the femoral nerve damage is not so bad. Still, the short-arc leg lift exercise is impossible for me. Not clear why.
Into the chair for my lunch, feeling good now.
And the afternoon PT session went very well. Walking, stairs, and a set of 10 exercises with no great pain or problems. And than a shower. So overall definitely an up day. I will spend the night here and get out tomorrow. Finally, this evening, a small bowel movement after nothing since Tuesday.
July 26, 2014: Saturday: discharge
Slept well. Feel good. Will surely go home today. Good PT session with Jen. Bend angle is 52° with help. Hematocrit back down to 30.6%. Likely causes of this loss of red cells is the thinning of the blood with IV solution (which affects this percentage measure) and the loss of red-cell-rich blood through seepage. The drain was taken out today, but there was some post-op seepage through the drain. A friend says that part of that is due to blood loss caused by the cut bone.
Yay: JB came by for long chat. PA Youngblood then certified me for discharge. He does not agree that the anesthesiologists’ recommendation of Lyrica and Celebrex is necessarily warranted. My quad function is there, but I get the sense it is less than they like to see at this point.
2:00 Home now. Yay. Now I must be careful not to overdo it. From one friend who had total knee replacement: “Follow carefully your medical team instructions. I made a bad mistake. 8 days after surgery I went for a 3-mile walk. I was so proud of myself. My surgeon reprimanded me as there was still a lot of hematoma around the knee. The bottom line: it took about 9 months to be pain free, attributed to my premature long walk.”
Yes, I will follow the protocol carefully. Played the piano a little. The sustain pedal works, but I need to put more weight/focus to get it to work than when normal.
Evening: A little tired. A phys. therapist is coming by in the morning. I do have oxygen here and I will use it overnight.
July 27, 2014: Sunday: first day at home
Della Crone is coming over this am for first PT session. I do have lots of questions, like whether there is a goal for angular movement at knee at time of first visit to Dr. C. Night was restless, a little painful but only a little. I used oxygen at 2 liters during the night.
Excellent PT session in the sense of covering a lot of ground. All goes well except the quad. It is firing, but not strongly. A goal for the Dr C meeting would be range of motion of 65° or more. I think I can make that. I just cannot even start a leg lift straight up. But if I lie on my side and aim it at a 45° angle, I can do it.
July 28, 2014: Monday: Slow day
Playing the piano in the morning I found I could concentrate much longer. Perhaps due to a rising hematocrit: more red cells. I slept with one liter oxygen flow. Midmorning CPM after exercising: I had it rising to 55° with no problem, with short stretches at 60 or more. Good.
Late afernoon phone call from anesthesiologist JB following up. He feels now that the tourniquet time was not long enough to do any serious damage and that, given progress of last few days, my story is close to normal. Says that discontinuing the Celebrex is sound.
Every evening my temperature is up to 99.5° or so. That is normal for healing of such a wound; but it sucks out energy. And the knee is painful after all the exercises, but in the morning it is quite calm.
July 29, 2014: Tuesday: Hallelujah! Electrical miracle.
Hard to get a good night’s sleep. I have been taking oxygen, but think I will stop now. The use of the pedal on the piano is a good exercise as it flexes the leg.
PT at 11:30 am. On Sunday my friend Bob P. brought over an EMS (Electrical Muscle Stimulator). Della’s eyes lit up when she saw it. It took a while to calibrate it away from a painful level. But then, with it running in 10-second bursts, we could see the quad sets being much stronger. So then I tried the short-arc leg lift and the full leg raise, two exercises that I could not previously do at all. And it was like one of those religious healing ceremonies: “RISE UP, LEG, RISE UP!” And it did. For both exercises. “AMEN”. And then after disconnecting EMS I could still do them, though less well.
Range of motion up to 61°. Now using PCM machine at 70°.
July 30, 2014: ONE WEEK. Wednesday: Drug allergy?
Last evening my temperature was100.2°. This morning it is 98.6°. I slept without supplemental oxygen last night; no problem. Full set of exercises morning and afternoon. And a shower. And change of dressing.
Now I find lots (50) of small red dots, mostly on my back. I called the surgeon’s office and they had no idea what could cause it. Googling “skin rash” with some of my drugs leads to lots of stuff. Maybe I will ease off the pain meds. tonight. A nurse from the hospital just called —routine—and of course I told her all this. She says cut out the pain meds (Oxycontin) if I can, then if no relief, call VSO to see about cutting down the blood thinner (Xarelta).
July 31, 2014: Thursday: Drug test
Took no oxycontin last night. Pain increased dramatically. Took it in the morning. Called VSO and spoke to Matt who said that red spots on back or thigh are not a great concern (and are common with oxycontin) so long as they do not worsen. Stick with the drug program; take Benadryl if they worsen. Clearly pain meds are still needed so I can do the PT at the right level.
Good PT session, my last with Della. She observes that the out-patient PT will give me more access to more specific machines. We did not do any electric stimulation today. Angle now up to high 70s. Can do 85 on the CPM machine. Goal is a right angle by the weekend.
Aug. 1, 2014: Friday: Right angle approaches
Usual restless night. PCM machine up to 87 degrees. Still cannot get leg even 1 mm up in a straight leg lift. Bent leg lift works. Two sets of exercises as usual. Very close to 90° now. Red spots are stable. I am still taking two oxycontins each day.
Aug. 2, 2014: Saturday: First excursion
The usual restless night. Forgot to take my pain med. until noon. But I still got through the morning exercise session. Range of motion up to 88°. Still no straight leg lift. The trip to the Breckenridge Music Festival concert went well. The piece by Friedrich Gulda (Concerto for Myself), pianist Lisa Smirnova, was superb: best piece I have heard this summer. I feel like a fledgling: Very close to taking my first steps without crutches.
Aug. 3, 2014: Sunday: Quadricep breakthrough
In my morning exercises I could perform 10 leg lifts from a horizontal position. Before this I could not raise the leg even one millimeter. This is a huge breakthrough, and surely means that there was no serious nerve damage. It must be that the swelling has prevented this exercise, and the swelling goes down all the time. And now I am using the CPM machine up to 94°.
Today we drove our house guests Christine and Scot high above Leadville, where I waited in car while they hiked to the top of Resolution Mountain. Looked for mushrooms. Nothing.

Aug. 4, 2014: Monday: A Right Angle
PT at home with Karen Gage today. She got flexion up to 90°. Extension is still 8° off of horizontal, so that is slow going. I am not ready to try walking with one crutch; need to perfect the gait using two crutches.
And I can now start on the rowing machine. Today: 1000 m in 6:21.
Measured my height carefully. 5 feet, 6 and 13/16 inches, just over 5′ 6.75″. Since I have called myself 5’6″ in recent years, that’s nice. Of course, I have not gained 3/4 of an inch. Yet by straightening my right leg the surgery will have made me a little taller.
Aug. 5, 2014: Tuesday: First followup with Dr. C.
Excellent visit with Dr. C. today. Staples removed. Blood-thinner discontinued, though I will take one normal aspirin per day for a month. The pressure socks are discontinued. Schedule: Expect to drive four weeks post-op. Expect to slowly go from two crutches to one, then to a cane. No rush. Next goals are to have range being 0 to 120 degrees. Pre-op my extension range was 4°, but it should come down from current 8° to 0° slowly.
He commented that he chose the size of the spacer—the plastic cartilage substitute—to be wide, thus leading to a tight knee. This might slow down the recovery of range of motion, but in the long-term will be better for the sports (skiing) that are important to me. And he felt there was no nerve damage: quadriceps failure is quite standard for many days after this surgery.
At 10 pm there was plenty of pain. I took Oxycontin then, slept fitfully, and then woke at 3 to no pain. Presumably it is just because of the drug.
Aug. 6, 2014: TWO WEEKS. Wednesday: New physical therapy system; Rowed 1000 m in 5:59
Today I started a program of physical therapy at Howard Head. Good session. Eric agrees that I have 90° flexion but could get only 10° extension. I have a program of home exercises to be done three times a day.
I feel close to being able to walk with one crutch.
Aug. 7, 2014: Thursday: Rowed 1000 m in 5:38
I can now move around on one crutch, though my gait is much better when I use two.
I sometimes add things to previous links. In the first link of this knee blog I added an Xray of my knee pre-op. It is heartening to compare the spacing in the knee in that Xray to the spacing post-op!
Aug. 8, 2014: Friday
PT coming up at noon. I surely would like to see my angles improve. Getting to a right angle was no problem, but progress beyond that seems nonexistent.
Well, the range is not improving. I need more aggressiveness in the exercises and more time on the CPM machine. My extension was measured at 8° which is better than the 10° from Wednesday. I am now on the CPM with max at 100°, though that is not a measure of the true angle. But it is still a good exercise.
Aug. 9, 2014: Saturday: Driving!
Just heard about someone who had knee replacement recently and developed some sort of infection requiring a second hospital stay. So that does happen. Drove around the block for the first time. 18 days post-op. No problem.
Aug. 10: Sunday: Discontinue pain meds
I took no pain meds last night and slept well. And none this morning either. CPM machine up to 115°.
Aug. 11: Monday: Good night
Got through the night with usual wakefulness, but did not go to the bathroom during the night. That is a first since the surgery. Wonder why? Less fluids from swelling decrease? I feel close to walking without crutches, but gait is much better with them. And no pain meds now.
PT feels I should go to five days a week, not three. Extension down to 7° today. Dr. C. comments that the thick plastic piece should affect extension, not flexion. And he says that gains here come in fits and starts. Flexion seems stuck at 90°. PT also feels that taking an oxycodone prior to PT is a good idea.
Aug. 12: Tuesday: Bad night
For whatever reason, a bad night, with a lot of pain. Hardly any sleep. Maybe the hard PT session? Combined with house guests (Peter and Gail Gagarin and JJ Cote) and a late exercise session. Should have taken a pain med, but I felt fine. PT suggests five days a week not three, and taking a pain med in the house before PT. Sure.
Very good PT session. PT sees strong improvement in extension, though we did not bother to measure. This confirms my general sense that I have been making progress on extension. And flexion is past a right angle. A few minutes were spent with the electro-stimulator on the quadricep. PT also thinks my coming cold turkey off the pain meds was a bad idea. I drove myself there and back with no problem.
Rowed 1000 m in 5:18.
Aug. 13: Wednesday: THREE WEEKS: Three digits flexion
Another poor night. Was able to go to early morning piano lesson in Breckenridge and focus and play. Excellent PT session. Flexion jumped to 100°. And we tried a new (self-) torture machine: the Extensionator.
Aug. 14: Thursday: 102° flexion
Got flexion to 102° today at PT, possiby a little more.
Aug. 15: Friday: Machine trade
The swelling is modest so I turned in the GameReady ice machine I’ve been using since surgery. But I replaced it with a self-torture machine called the Extensionator. Warning: Never confuse with an Extendinator!
Good PT session with flexion up to 105° and extension down to 5°, both solid improvements. These days for pain meds I take one oxycodone before PT and another before sleeping.
And back to rowing machine today: 1000 meters in 4:59; a 19 second improvement over Tuesday.
Dinner at Dave and Janet’s. Alcohol makes me a little dizzy still.
Aug. 16, 17: Saturday, Sunday: 1000m row in 4:49 Homeowners’ Meeting(s) Saturday. Lots of exercises all weekend. Rowed 1000m in 4:49 on Sunday; of course each time has more flexion, making it easier.
Aug. 18: Monday: 110° flexion, 1000m row in 4:39.8
Good long session today at PT. Lots of progress. Eric thinks I am ready to move down to one crutch. Flexion is up to 110°. My walking gait is improving. And Eric gives me the green light for a San Francisco trip over Labor Day weekend. And I can now get the pedals around on a normal stationary bike (as opposed to recumbent), at least if the seat is high enough. I have some sensitivity in the shin below the knee; Eric says that is because there is not much room there, and so the swelling causes small pain in that area.
We removed a few steri-strips, but the scar is still not fully healed, so we replaced them with new ones and should probably leave them on for another week.
Aug. 19: Tuesday. I can now get my legs around a revolution on a stationary bike, and a friend will loan me one for use here at home. At PT we looked again at part of the scar: parts are healing well, others are better covered for a while more. Went for a walk to the end of the street.
Aug. 20: Wednesday: FOUR WEEKS: 3° extension; 1000m row in 4:36
Piano lesson in a.m., then long PT session in the afternoon. Extension is now down to 3°. Since, pre-op, it was about 4°, this is a breakthrough. I imagine there will be no problem getting to 0. Walking with one crutch is fine. We are now introducing some new strengthening exercises aimed at the calf and quadriceps. I now have a stationary bike at home, but I cannot quite get around one revolution on it.
Aug. 21: Thursday: 113° flexion. Very tired after two-hour PT session in am. Nap in pm. We looked at the scar which is healing well, but then put some new steri-strips on. I have a little clicking in the knee. It seems minor and I think/hope it will go away.
Aug. 22: Friday: Good night; 1000m row in 4:32. For the first time in a month I could stay in bed all night. Good PT session as the extension continues to improve, as it approaches 0. I believe now I have more extension than I had pre-op. I am using one crutch, but it feels like I am close to walking with no crutch. No pain meds during the day in past few days.
Aug. 23: Saturday: ONE MONTH. Mushrooms! Joan and I went mushroom hunting today and found about ten perfect porcini. Of course I could not go very far from the car, but I hobbled around on one crutch and sniffed a few out. It did exhaust me.
Aug. 24: Sunday: Is there an average timeline for recovery?
Well, I had to look online to see what typical timelines are. Found this:
http://www.healthline.com/health/total-knee-replacement-surgery/rehabilitation-timeline
Many things don’t make sense to me, but I suppose everyone is different. The web site says that on discharge from hopsital one should have 90° flexion. I had about 30˚. Then they say by week 11 you should have 115 degrees, something I was close to now at 4 weeks. It also says 90° is a goal by week 6. Well, I am sure there is a lot of variation and I feel like I am having reasonable progress.
At Mil Plant’s 90th birthday party today I ran into a woman who had both knees done (7 years apart). She is very happy with the result.
Aug. 25: Monday: Extension trumps flexion
Now I can get around with a cane instead of a crutch, and perhaps even without a cane. Today’s therapist said that it was important to work on extension even though I am close to 0˚. After 6 weeks it becomes hard to make extension progress, while flexion progress can be made for months.
I have a bike on a stand here now thanks to Katie, but I cannot really get around one cycle yet. On the stationery bike at PT I was able to get around at height 5, whereas previously I needed height 6.
I can walk a bit with no cane or crutch, but it is tiring.
Aug. 26: Tuesday: More extension
Good PT session, working hard on extension. I am very close to 0° extension. Lori says it is a little behind the usual curve for this, but there are probably reasons (large plastic insert; pre-op was only 4°). We are of course now asking the insurance company for more than the original budget of 18 sessions. This is my 14th session.
Aug. 27: Wednesday: FIVE WEEKS: 2° and 115°
Good PT session as always. Scar looks good. There is always swelling and Eric says that will be with me for a while. The goals are 0° extension and 130°. A native knee gets 145°. Probably I had flexion of 135° pre-op.
Aug. 28–Sept. 1: Thursday–Monday: Excursion to California
Joan and I are going to California for a few days for a family visit. My walking is improving, if slow. I am taking the crutch with me. The new knee sets off the metal detector. So I guess, in future, it is pointless even going through the metal detector.
Arrived SFO no problerm. I’ve been told that exercises and PT are my “job” for this season. While these 5 days are a vacation from PT, I have to work hard to keep the exercise regiment going. The 7-inch scar is now completely healed.
Sunday: A nice one-mile (or close) walk high on Ridgecrest Rd. Felt good.
Sept. 2: Tuesday: Followup #2, SIX WEEKS. I can now walk without any device.
Good visit with Dr C. and Matt V. Everything looks good. My progress is slower than some because of the history: injury vs. normal arthritis progression. Bottom line: everyone is a little different. Alignment looks perfect.
Clicking: Two types: on certain twisting the metal parts will always click. On normal walking, there might be some patellar clicking now, but it should go away, especially with improved quad strength.
Goals for the next appt. in six weeks, Oct. 15: Range of motion should be 0° to 130°.
Matt suggests rubbing sunscreen into the scar.
Possibly I will need PT for six months to develop strength and keep working on the range.
Dr C. observes that a bike is much better exercise than walking at this point. I can now ride the bike at home and will do so regularly.
Sept. 3: Wednesday: Four Beautiful Porcini
Joan, Dave Blakeslee, and I drove to a high point where I have found piles of porcini before. Found only four this time, but they were all beauties. I walked about two miles. I put in some time on the stationary bike, and will now do much more of that.
Sept. 4: Thursday: Extension. Good session with Eric today as we worked only on extension. He “scraped” away some scar tissue with a metal tool. I did a 20-minute session on the Extensionator.
Sept. 5: Friday: 1°. Measured 1° extension at PT. Woke up this morning with a feeling of real improvement. Swelling down. Rode bike at PT for 15 minutes at seat height 3 and 4, after being able to do only 5 and 6 last week.
Sept. 6: Saturday: Rowed 1000m in 4:28.6. Lowered bike seat a bit more. Easy to maintain 60 strokes per minute. Then rowed 1000 m in 4:28.6. Heart rate up to 141.
Sept. 7: Sunday: 118° Flexion. I think I can get to 118° on my own with a wall slide. I did a geometrical analysis on the relationship between distance moved and flexion angle. Fun.
Sept. 12: Friday: Done with Extensionator; 0° Extension reached
A quiet week….I mailed the Extensionator back this morning. And at the PT session Eric got me to 0° extension, a major goal. Walking and standing feel much better now. Also sleeping better.
The problem is that just because a straight leg is achieved at PT does mean my leg is straight when I walk. But it is getting there. We have not worked on flexion at PT for two weeks, but home exercises continue and I think I am near 120°, with 130° being the goal.
I can now pedal away on Katie’s bike-on-stand at 60 rpm or more comfortably.
Sept. 13: Saturday: Rowed 1000m in 4:24.
But my HR went up to 145 and took a while to get down. Out of shape! I had biked 15 mins hard prior to rowing.
t noon I walked a little over two miles on the Dam Recpath at 20 minutes per mile for first mile, sloer for second. Pleasant.
Sept. 15: Monday: One leg balance
Today I could stand on the right leg, on a piece of rigid foam, for three minutes without using the left to touch the ground or to touch the top of the right foot. In short, a pure 3-minute balance. I think success here is related to continued quadricep development.
Surprise: I just learned of a research project using ideas similar to my square wheel work (and citing my paper) that uses spiral shapes to make a better type of crutch and also orthotic. Interesting.
Sept. 17: Wednesday: EIGHT WEEKS. Rowed 1000 m in 4:19.8
Flexion improves so that the rowing machine feels normal range now. Of course, the quads are still weak. Heart rate up to 147 on this row. And I am biking using the larger gears now (stationary), maintaining 60 rpm.
This fast row is a little hard on the knee at that pace. I should now go easier.
Sept. 18: Thursday: Full Range. With Eric’s help at PT I now have a range from 0° to 130°, which is what Dr. C. wanted to see by Oct. 15. So I think ultimately I will get past 130°. Pre-op, loosely measured, I was 125-130 flexion. I recall Dr C. saying the I might get a couple extra degrees, and I seem to be on track for that.
Sept. 19–22: Extension
Standing on one leg with eyes closed: right leg: 12 seconds. Very difficult. Left leg: About 30 seconds. Most often when I try this on the right leg I last for about 3 seconds.
Extension is 0 with Eric’s help, but when walking it is not 0. So we are working on getting it straight all the time.
On the 21st I played Debussy’s Arabesque in a recital and did well. It was my best performance in three times at these parties.
Sept. 23: Tuesday. Two Months Out (9 weeks): A First. I slept through the night, from 10:30 to 6 without waking. This was the first time that happened since 7/23.
Sept. 25: Thursday. Both Dr. C and Eric assure me that progress is normal. I tire easily on walks of a half-mile at 20 minute mile pace.
Sept. 27: Saturday: One Mile. Walked one mile around the neighborhood, small hills, in 18:16.
Sept. 29: Monday: One Mile. Same one mile walk in 17:08, well faster than two days ago.
Sept. 30: Tuesday: One-Leg Stand. One leg, eyes open: can now do three minutes fairly easily.
Oct. 1: Wednesday: TEN WEEKS I went a little too hard on the bike yesterday in high gear. Knee a little stiff today. Could stand on one leg with modest head movements for 3.5 minutes.
Oct. 2: Thursday: One mile walk in 16:22.
Oct. 3: Friday: One-legged stand: 4 minutes. And a 2 mile walk on the dam in 33 minutes. 16+17. Felt good.
Oct. 5: Sunday: One mile in 15:58. One mile in the nieghborhood (hilly) in 15:58.
Oct. 6: Monday: One mile in 14:32. One mile in the nieghborhood (hilly) in 14:32; after morning PT session. Eric suggests RPM of 70–75 with good resistance on the bike.
Oct. 8: Wednesday: ELEVEN WEEKS: 1.33 miles @16:05 pace
Oct. 9: Thursday: Proof of Straightness. With overpressure the leg straightens to 0°. Also did some one-legged easy squats today.

Oct 12: Sunday: Rowed 1000 m in 4:31.5. Felt out of shape. Should row more.
Oct 15: Wednesday. TWELVE WEEKS. Doctor Visit.
A visit to Dr. Cunningham went well. I am probably a little ahead of an average timeline. The little twinges I get are likely due to patellar tracking issues, that in turn are related to the weaker muscles. So building up the quad is key now. Basically all goes well. I will see him again in three months. After that, if all goes well, it might not be for 10 years. He says an X-Ray after five years will likely show little and so is not necessary. Some people stop PT at this point, but I will carry on for another month.
Oct 19: Sunday. Three-mile trail walk.; 650 ft climb.
Oct. 22–25: Travel to Champaign for Conference. The two flights on Wed. seemed to tire my legs, but I was fine on Friday, and went for a 1.8 mile walk on Friday.
Oct. 27: Flexion measure. Flexion measured at 125° at PT, but I think I had 130 earlier, so it was not as aggressive as I think it could be. Walked one mile (on the watch, so accurate) in 15:20. Hilly. Felt good.
Oct. 28: One mile, hilly, accurate, in 15:00 flat. Felt good.
Oct. 29: FOURTEEN WEEKS. Two miles. Flat. 30 minutes exactly.
Nov. 4: One mile. 14:25
Strong workout at PT. Two times 50 on the shuttle with 5 straps after doing 100 with 6 straps (the max). Then a good 10 minutes at max incline on the treadmill. And a solid 1-mile hilly accurate walk in 14:25, by far my best.
Nov. 5: FIFTEEN WEEKS. Three miles at 14:55 per mile. Flat.
Nov. 7: Rowed 1000 m in 4:22. Need more rowing practice.
Nov. 9: Rowed 1000 m in 4:30. Backed off to ease heart strain. Walking continually improves.
Nov 13: SIXTEEN WEEKS
Went skiing near the house on light touring gear. No problems except a little on the long strides when descending gently. The balance exercises all help. At PT today flexion is at 130°. It appears that will be my maximum. Pre-op it was vaguely measured at 125-130, so this is fine.
Nov 19: SEVENTEEN WEEKS: Final Strength Testing
Yesterday I did a solo ski tour at Vail Pass. Going up the Shrine Pass Road was fine. Coming down: the weakness was evident in my right leg. Hard to commit to the braking effect of a turn on the well packed road on the right side, so I was sore at the end.
I wondered what the total cost of this surgery was. I called the insurance company. By far the largest item was the payment to the hospital of about $58000. The other large items were the surgeon’s fee of $6000 and the anesthesiology fee of $2900. I am not sure about the post-op PT cost. There were other small items. So a ballpark estimate is $68000. This seems in line with what appears in the news as the cost of a total knee replacement.
Today was the last of my 38 visits to Howard Head Physical Therapy. Eric did some strength testing. The results:
Involved vs Uninvolved Leg:
Knee Extension: 91.2%
Knee Flexion: 75.5%
Hip ABD: 90.1%
Hip Extension: 99.9%
Hip ER Prone: 98.2%
Hip Flexion: 105.3% (!)
These are all quite good. I wonder if that 75% is because right leg flexion has worse than left for many years pre-op.
The hamstring-quad ratio was 50.5% in left leg and 41.9% in right. Eric thinks these should be closer to 70%.
I will likely do these again in January sometime, with a goal of getting the knee flexion to 90% and improving the hamstring:quad ratio.
Nov 21: Walk one mile, hilly, 13:47 (prev. best = 14:25 on this route).
Nov 29: 18 WEEKS. Skiing regularly now. All goes well.
I have not yet tried skate-skiing or alpine touring. But classic skiing goes well. Out for almost 3 hours today in powder snow near French Pass.
Dec 9: 20 WEEKS.
Just continual improvement now. Nordic skiing feels easy and I am able to spring a little. So I think it is fair to say that the whole business has gone as well as hoped.
Dec 18: 21 WEEKS.
Continued nordic skiing, both skating and classic. This morning I skinned about 2000 feet up the Keystone Ski Area for my first day on the big AT skis. All went well.
Jan. 27, 2015. 27 weeks. Last doctor visit; notes for future
All went well at today’s visit, my last, with the surgeon Dr. Cunninghan. He says that taking an X-Ray to check on things is reasonable in 10 years, and perhaps every 2 years thereafter. I still feel swelling and stiffness after exercise, but that is normal. January has been a fine month for nordic skiing and I have been skiing daily, even getting some good times on my little time trials. So all in all a great success. No regrets.
Future Notes:
Take antibiotics before dental work, or other procedures, for two years from surgery date (to July 23, 2016).
If I injure my skin and any sort of infection develops, treat medically as needed to minimize chance of knee infection.
My left knee shows some crepitus; strengthen hamstrings and stretch IT band to improve it.
Feb. 2015: Racing again
I have now done two nordic races: 10 km and 44 km, both in classic style. The latter was in slow conditions (the Leadville Loppet; cold and snowy) and took me 4:59. A bit of swelling/stiffness near the end of the race, but it had minimal impact on my ability to ski. In my age group I was third in the short race and first in the long. So all in all I have to be very happy about how the recovery has gone.
April 2015: 9 Months. Backcountry ski trip to Canada
The knee performed well on a backcountry base-camp ski trip to a remote region of the Canadian Rockies. Details at http://stanwagon.com/wagon/canskiing/Valenciennes.html. There was some soreness and I was a little slower than my young friends, but I never needed a rest day.
July 2015: One Year. Climbing trip to the Selkirks
Spent a week at Houston Lake (near Battle Abbey in the Selkirk Mts. of B.C.) during which David Nebel and I climbed Moby Dick with guide Pierre Hungs, and then Pierre and I did Proteus. These took 13.5 and 12.5 hours, respectively. The second had more rock climbing and my knee was a little stiff at the end. Hoping the stiffness disappears, as I expected it to after a year. But these were very strenuous climbs. Trip report here.
Nov. 7, 2015: First ski day of new season
After a summer of running and hiking it is wonderful to get back to sliding. A few days ago I visited my physical therapist to discuss a few things. There is some scar tissue above the kneecap. It is not really limiting me, but it would be nice to have it decrease. He gave me some exercises, etc. We also discussed activities I should or should not be doing. There is disagreement about running, but it seems that mild and slow running is probably fine. I should have an XRay in five (or four?) years to make sure everything looks good.
I did one fast 15-minute run on blacktop up here (8700 feet) to try to estimate my VO2 max. I averaged 9:07 pace and so it seems that my VO2 max is about 44. That is good.
Feb. 4, 2016: Report
Ski season has been great and I have been doing less skating and more classic skiing. The knee is not perfect, but as far as skiing goes I typically do not think about it at all. I finished 92 out of 112 in the Stagecoach Classic 30 km race from Devils Thumb to WInter Park (2:54) and felt good about my race (bad wax was a problem for a large part of the race). There is a little stiffness above the joint (scar tissue?), but no other problems.
Oct. 1, 2016: Report
Now well over two years out. This past summer was much better than the one-year-out summer in terms of fitness. There is a small amount of stiffness at the top of the knee (scar tissue?) and occasional very slight inflammation pain at rear of joint, but nothing like before. I am able to hike fast and run fairly well, with no problems of any significance.
Oct. 23, 2016: Report
I did my first backpack in six years to Faraway Arch in Cliff Canyon. The new knee behaved very well. Now some soreness in the other knee (10/25/16). Seemed like a cartilage issue so of some concern, but by 11/4/2016 it was much better. By 11/16 it seems quite normal.
Dec. 13, 2016: Report
Generally it is fine. Skiing seems fine. But when I am on my feet all day, exercise and then some cooking, say, by late afternoon I am getting a pain that seems very similar to the inflammation in the popliteal area that was my problem pre-replacement.
Sad news: In November 2017, physical therapist Eric Dubé died of a heart attack while mountain biking in Moab, Utah.